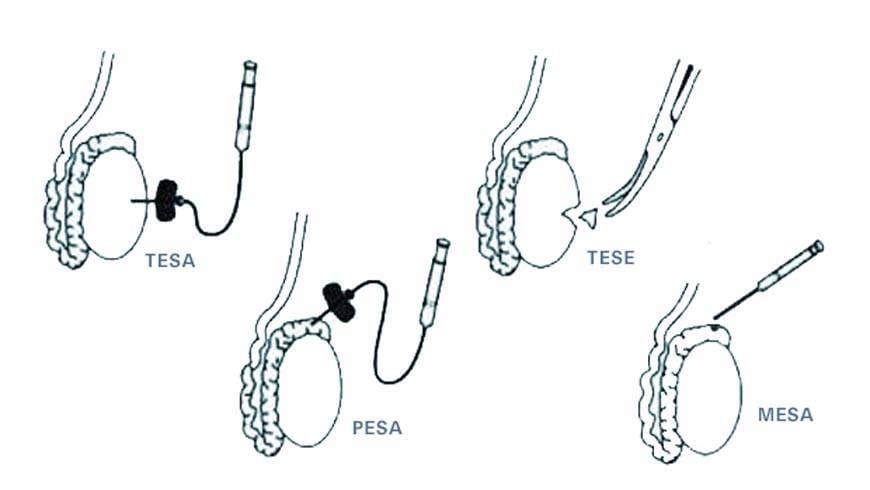
The condition in which there is no sperm in the semen is called azoospermia. It results from blockage/obstruction in the sperm ducts or from dysfunctions in the testes where sperm is produced. Its treatment is micro-injection. In this treatment, sperm collection is done by surgical procedures known as TESA or TESE by the urologist. About 5% of couples applying IVF centres for treatment are treated in this way.
TESA (Testicular Sperm Aspiration) When there is no sperm in the semen taken from the male due to blocked sperm ducts (obstructive azoospermia) or because there is very little sperm production, sperm cells are collected by aspirating the tissue/sperm by inserting a needle into the testicles.
The operation is done under local anaesthesia and the patient can return to his daily life on the same day. Mature or developing sperm retrieved with this method are used in ICSI (microinjection).
TESE (Testicular Sperm Extraction)
When sufficient results cannot be obtained via TESA or when there is a significant lack of sperm production, a piece of tissue is removed (biopsy) by a surgical operation. The operation is done under local anaesthesia and the patient can return to his daily life on the same day. This procedure involves extracting small pieces of tissue of the testes through s close study under the microscope. Using a surgical microscope helps determine areas of tissue where the chances of finding sperm is higher. Moreover, intrusive damage risk to the veins feeding the tissue will be decreased to the minimum. Removed tissue is put under closer analysis under the microscope. When sperm is found, various preparation procedures are started for ICSI (microinjection).
Micro Tese Procedure
Men suffering from azoospermia and cannot have children because of this can overcome this problem with “microscopic testicular sperm extraction” known as “micro tese”. In cases which do not involve obstruction (blockage in the tubes), sperm production in the testes is none at all or at a very low level in some areas. While some tubules do not produce any sperm, some others may do some. By use of a surgical microscope, areas containing sperm can be identified easily and sperm can be retrieved from males who do not have any sperm in their semen. Under anaesthesia testes are partly dissected by incision and analysed under the microscope. Because the procedure involves less testicular tissue extraction, areas with more sperm production can be identified easily and since tissue retrieved is small, more pieces can be obtained from various parts. These pieces are cut in and sperm spread in the canals or attached to the canals are then picked up and used in microinjection in the laboratory by an embryologist. The scan and monitoring of the testes by a microscope increases the chances of finding and collecting more sperm. Another important point is that this method causes less tissue loss compared to older methods. Thus, the testes are damaged as minimally as possible and procedures which might lead to decrease in testosterone levels in the blood are avoided in this operation.
Who can benefit from it? Patients who have had conditions such as…
- The absence of sperm ducts (canals) by birth
- Obstruction in sperm ducts
- Hormonal factors
- Genetic reasons; genes responsible for sperm production are on the Y-chromosome. A condition in these genes affects sperm production.
- Medication, especially some medication used in cancer treatment, can prevent sperm production permanently
- Infection (post-mumps)
- Radiation; especially exposure to radiation due to cancer treatment can prevent sperm production permanently
How is the procedure done? It is a procedure done under anaesthesia; thus, it is painless. By use of a microscope, tissue samples are taken from at least 4 different parts of both testes. Through a series of procedure, alive (healthy) sperm cells are separated. These are used in microinjection. In testis, a biopsy sample is taken from only one part of the testis. However, there might be sperm production on other parts. Thus, if sperm cells cannot be found through testis biopsy, sperm can be obtained via TESE from patients. There is a risk for the female partner to start treatment unnecessarily if there is no sperm count. Thus, sperm cells obtained via micro tese are frozen and stored, then, the patient starts with the treatment plan. Freezing and storing (cryopreservation) doesn’t affect sperm quality. Besides, storing makes it possible to have a second IVF treatment without going through Tese surgical procedure. Things to consider “The last 6 hours, prior to the operation, nothing should be consumed (eaten or drunk, not even water)” Clean (Shave) the body part to be operated on and have a bath. “Bring large/loose trousers or sweatpants, since clothing might cause pressure on testicles; thus, pain after the operation.” You will be discharged in about 1-2 hours after the operation. 3 hours after the operation, you can start having liquids. 5 days after the operation, you can have a bath. Do not have sexual intercourse for one week. If you feel pain, you can take painkillers “Contact your doctor if there is rash, swelling or bleeding on the area” Since self-dissolving stitches are used in Micro TESE, there will be no removal procedure for the stitches. The stitches will dissolve in 7-10 days There is a chance of not being able to obtain sperm cells after the operation. This risk depends on the reasons behind it. The chances of finding sperm are higher in a patient which has obstruction in his ducts compared to a patient who has hormonal or genetic problems. There might rarely be infection or bleeding on the area after the operation.